Recent groundbreaking research has established a direct cause-and-effect link between mitochondrial dysfunction and memory loss associated with neurodegenerative diseases such as Alzheimer’s and frontotemporal dementia. For the first time, scientists have shown that targeting mitochondria—the cell’s energy-generating “powerhouses”—can reverse memory impairment in animal models.
The Key Discovery
Researchers from France’s Inserm, University of Bordeaux, and Université de Moncton in Canada created a novel tool called mitoDREADD-Gs. This engineered receptor is inserted into the mitochondria within neurons. Activation is achieved by administering a lab-made, harmless drug (clozapine-N-oxide, CNO), which ramps up mitochondrial energy production—but only inside the mitochondria, with subcellular precision.
In mouse models of dementia, activating mitoDREADD-Gs restored normal mitochondrial function and reversed memory deficits within hours.
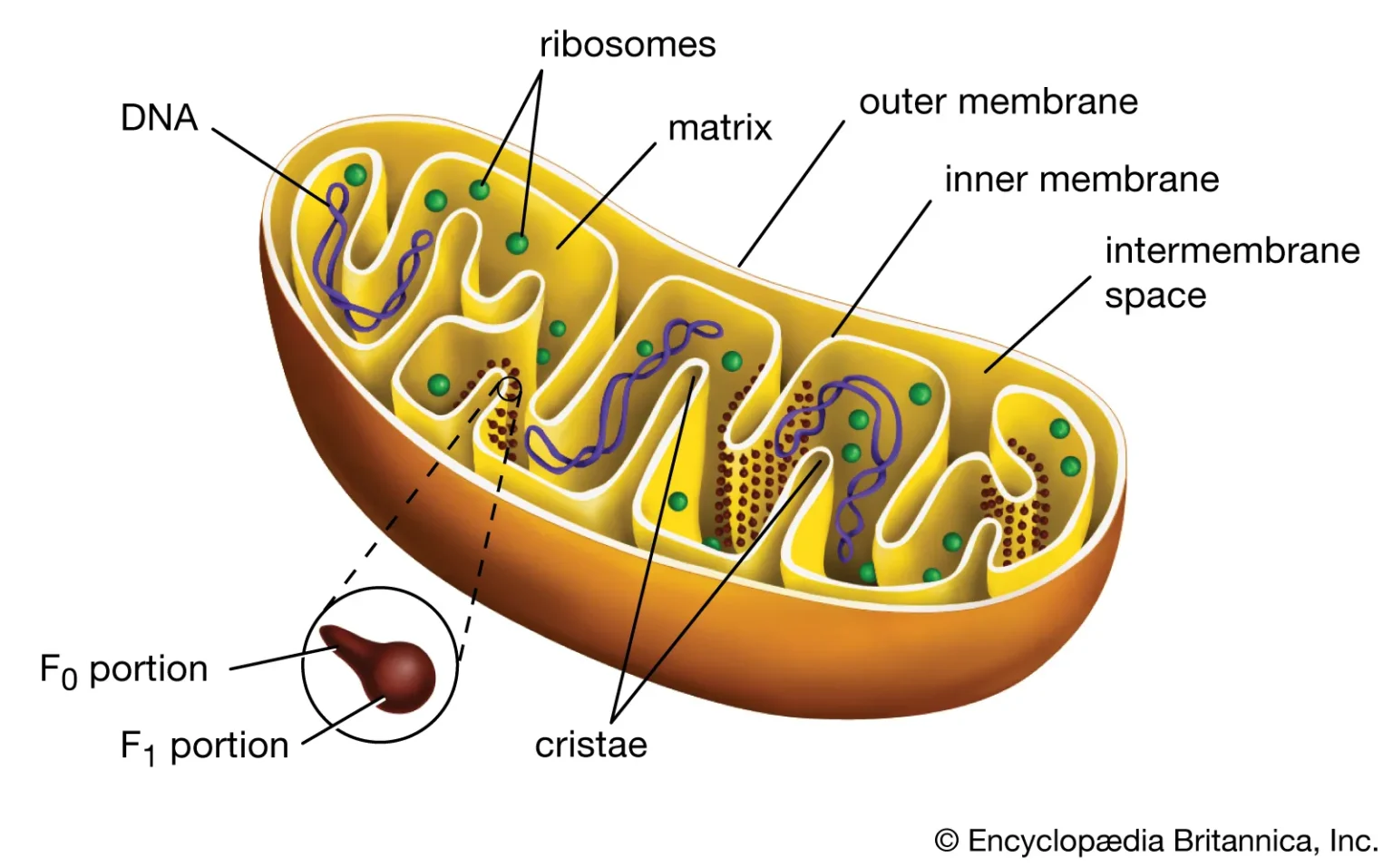
This mechanism works by increasing the mitochondrial membrane potential and oxygen consumption, both markers of robust energy production necessary for proper neuronal activity and memory formation.
Why it Matters
Previous research could not prove whether mitochondrial dysfunction caused symptoms or was simply a byproduct of brain disease. This study shows mitochondrial decline directly drives memory loss—restoring their function can quickly reverse these symptoms, as long as neuronal networks are still intact.
The findings highlight mitochondria as a promising new therapeutic target for slowing, preventing, or even reversing memory loss in neurodegenerative conditions.
Limitations and Outlook
These results are currently limited to mice. Bringing this precise genetic engineering technique to human patients faces major safety and practicality hurdles, especially in advanced dementia where many neurons have already been lost.
The improvement in memory is temporary—the boost fades when the drug wears off, so ongoing treatment would be needed.
The study opens “major avenues for further research” into mitochondrial stimulation as a way to treat energy-impairment related brain conditions.
Supporting Evidence
Other studies have found that compounds supporting mitochondrial health—such as acetyl-L-carnitine (ALCAR) and lipoic acid (LA)—can improve memory and reverse signs of aging in animal models by restoring mitochondrial structure and function, further reinforcing mitochondria’s role in cognitive health.
In summary: Scientists have developed a precision tool that directly increases energy production within mitochondria, reversing memory deficits in mouse models of dementia. This offers compelling proof that mitochondria play a causative role in memory loss—and that therapeutic strategies to restore their function could transform dementia treatment in the future.